Silent Threats in Healing Spaces: Understanding and Preventing Hospital-Borne Infections
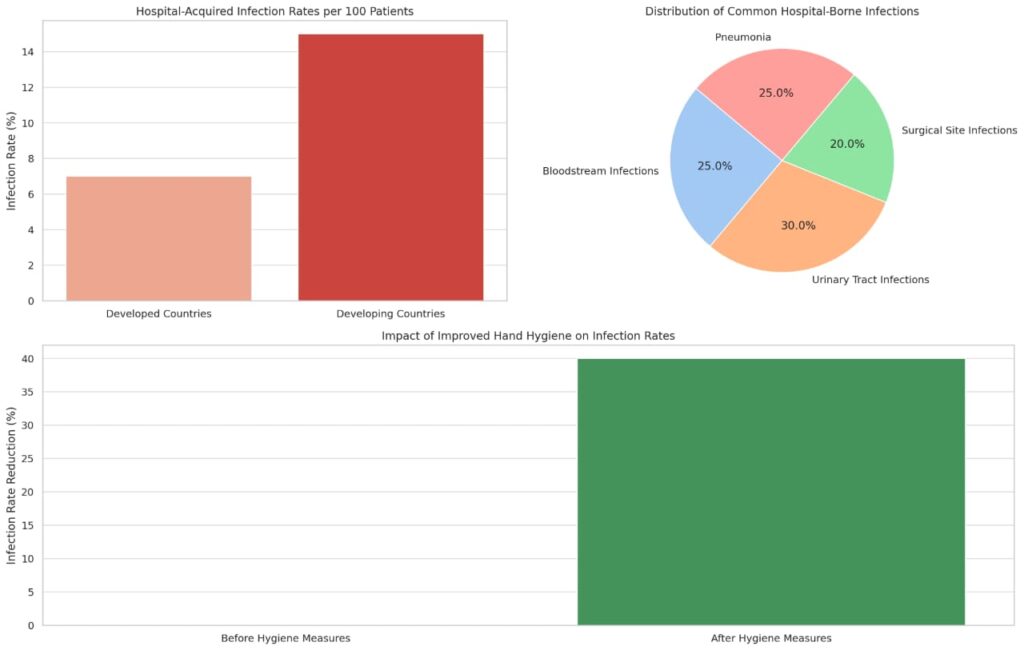
Hospitals are often seen as safe havens—places where people go to get better. But what many don’t realize is that hospitals can also be breeding grounds for a hidden danger: hospital-acquired infections (HAIs). Also known as nosocomial infections, these are infections patients acquire during their stay in a hospital or other healthcare facility, and they are not related to the condition for which the patient was initially admitted. According to the World Health Organization (WHO), out of every 100 hospitalized patients, 7 in developed countries and 15 in developing countries will acquire at least one HAI.
Hospital-borne infections can take many forms. The most common types include bloodstream infections, urinary tract infections (often from catheters), surgical site infections, and pneumonia (especially from ventilators). The pathogens involved are often resistant to multiple antibiotics, making treatment more difficult. The Centers for Disease Control and Prevention (CDC) has listed antibiotic-resistant bacteria, such as MRSA (Methicillin-resistant Staphylococcus aureus) and Clostridioides difficile, as major threats to global health due to their prevalence in hospital settings.
Why are hospitals—ironically, the places meant to heal—prone to such infections? The answer lies in a combination of factors. First, hospitals are filled with vulnerable individuals—those who are already sick or have weakened immune systems. Second, invasive procedures and devices (such as catheters and IV lines) provide direct pathways for microbes to enter the body. Third, inadequate sanitation, overcrowded wards, and lapses in hygiene practices can all contribute to the spread of infection.
The fight against HAIs begins with awareness and strict preventive measures. Hand hygiene is the single most effective way to prevent the spread of infections. According to a 2022 study published in The Lancet, improved hand hygiene practices among healthcare workers reduced infection rates by up to 40%. Regular disinfection of surfaces, proper sterilization of equipment, and isolating infected patients are also crucial steps. Hospitals must also invest in staff training and ensure adherence to infection prevention protocols at all times.
Patients and visitors also have a role to play. Being proactive—asking whether devices are still needed, ensuring doctors and nurses sanitize their hands, and following hygiene guidelines—can make a significant difference.
Hospital-borne infections are preventable, but only if everyone—medical staff, patients, visitors, and administrators—takes responsibility. In a space where lives are meant to be saved, there is no room for complacency.
Let’s stay informed, stay aware, and work together to make hospitals places of healing—not harm.